Spinal Cord Injury Update
Spring 2015: Volume 24, Number 1
Swollen Feet and Legs: Edema in SCI
By Shawn Song, MD, SCI Medicine Fellow, UW Department of Rehabilitation Medicine
Contents
-
What is edema?
-
Physical signs
-
Consequences
-
Treatment
-
Summary
What is edema?
Edema is swelling caused by too much fluid in your body’s tissues. Edema in the lower extremities—feet, ankles and legs— is a common problem among patients with spinal cord injury (SCI). It occurs more frequently in people with SCI compared to able-bodied individuals because paralyzed muscles are unable to pump blood that has pooled in the legs due to gravity back from the leg veins to the heart. As a result, blood collects in the legs, and fluid from the blood leaks out of the vessels into the surrounding tissue. This type of edema is termed dependent edema (because the legs are “dependent” or hanging down while sitting). While there are several other medical conditions that can cause lower extremity edema, dependent edema is the most common type among patients with SCI.
Physical Signs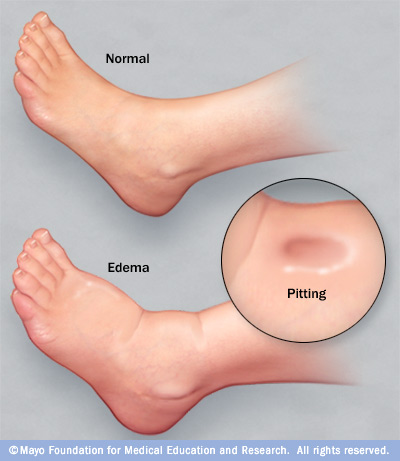
Though you can usually tell whether edema is present just by looking, legs can sometimes appear normal if the edema is mild. A reliable way to detect edema is by pressing a finger into the skin over the lower shin. If an indentation remains for several seconds after removing your finger (called “pitting”), lower extremity edema is present (see figure on right). You can also examine the skin under your sock – an indentation left by the sock is an indicator of edema.
If leg swelling is asymmetric (not the same in both legs), this may be a sign of a more serious medical condition. For example, blood clots in the veins of the leg, a bony fracture, or an abnormal bone formation called heterotopic ossification, can all result in new, asymmetric leg swelling and require immediate medical attention. You should always let your medical provider know if you have any new leg swelling, even if in both legs, since this may be a sign of a new or worsening medical condition.
Consequences
The major consequences of dependent edema involve the skin. Dependent edema, especially if long-standing, can cause the skin to become thin, fragile, and more vulnerable to breakdown. Significant foot swelling can cause shoes to fit poorly, potentially leading to pressure ulcers. If you already have a pressure ulcer, dependent edema can prevent or delay healing. Finally, dependent edema is a risk factor for infections of the skin of the legs, known as cellulitis. Be sure to seek immediate medical attention if you have edema along with new redness and/or warmth, since this may be a sign of cellulitis.
Treatment
Leg elevation
Elevating the legs reduces the effect of gravity and helps the fluid that has collected in the lower legs to drain back to the heart. The higher your legs are relative to the level of your heart, the faster fluid will drain out of your legs. For example, lying in bed with the feet at the level of your heart is generally better than raising your legs while seated. However, lying in bed is not always practical, so you can extend your legs from a seated position or perform tilt-backs in a power wheelchair at regular intervals to minimize fluid collection in the legs. Small studies have shown that elevating the feet by as little as 30 degrees for 15 minutes reduces the amount of lower extremity edema.
Precautions
- Take care to protect your skin while elevating your legs. If you are sitting down with knees straight and heels resting on a chair, make sure your heels are on a cushioned surface for no longer than 15 minutes in order to prevent a pressure ulcer.
- Another concern is the possibility of increased urine output as the lower extremity edema resolves. For example, if you have significant dependent edema and get into bed, the fluid from your legs returns to circulation, and your urine output overnight may be greater compared to during the day. You therefore may need to self-catheterize more frequently at night as a result of increased urine output.
Compression stockings
There are two main types of compression stockings—gradient and anti-embolism. Gradient compression stockings are the type appropriate for the majority of SCI patients. Gradient compression stockings are constructed so that the compression level is highest (or tightest) at the ankle and less at the top of the hose. This pressure gradient helps to minimize fluid collection in the legs and return blood to the heart. Gradient compression stockings come in different compression levels and can also be custom-made. There are also different lengths of stockings, from knee-high to thigh-high.
You should put on the compression stockings in the morning before getting out of bed, as your legs will have the least amount of fluid at that time. Make sure the stockings do not bunch or wrinkle as this can cause increased pressure over these areas. Consult a medical professional to determine the compression level and appropriateness of gradient compression stockings.
Precautions
- You should not wear compression stockings if you have peripheral artery disease (PAD). If there is any question of PAD, you will need to have a vascular evaluation including an ankle-brachial index.
- You should not wear compression stockings if you have active cellulitis of the lower extremities.
- If you are susceptible to autonomic dysreflexia, speak to your SCI physician before using compression stockings.
- If you have impaired hand function you will need to be supervised the first time you put on compression stockings to make sure you are putting them on correctly.
- Make sure to closely monitor your skin for evidence of irritation or breakdown when first using compression stockings and remove stockings at the first sign of skin irritation.
Medications
Diuretic medications, which help the body shed water, can treat some forms of edema. However, we do not recommend routine use of diuretics for dependent edema, as these medications can have unwanted side effects, especially related to low blood pressure.
Summary
- Dependent edema is a common problem among individuals with SCI.
- Dependent edema is caused by blood pooling in the leg veins, with fluid from the blood then leaking out of the vessels into the surrounding tissue.
- Potential consequences of dependent edema include fragile skin, pressure ulcers, and infection of the skin called cellulitis.
- New or asymmetric leg swelling may be a sign of a more serious medical condition and requires medical attention.
- Treatments include leg elevation and compression stockings.
- Compression stockings should be prescribed by a medical professional.
- Patients should closely monitor the skin over their legs for signs of irritation when elevating them or when first using compression stockings.






