SCI Forum Report & Video
Osteoporosis and Fractures in Persons with SCI:
What, Why, and How to Manage
By Jelena Svircev, MD, Assistant Professor at the University of Washington in the Department of Rehabilitation Medicine and staff physician at the Spinal Cord Injury Service at the Department of Veterans Affairs at the Puget Sound Health Care System. Presented on November 13, 2012.
If you have a spinal cord injury, you may be aware that you have a high risk of developing osteoporosis and possibly breaking a bone. This presentation will help you understand why this happens, what you can do about it and how to avoid fractures and their life-disrupting, painful and costly consequences. Watch the video or read the report.
Presentation time 60 minutes. After watching the video, please complete our two-minute survey.
You can also watch this video on YouTube with or without closed-captioning.
For a complete list of our videos, click here.
Contents
- About bones
- What is osteoporosis?
- How is osteoporosis diagnosed?
- Osteoporosis in SCI
- Screening for osteoporosis in SCI
- Treatment for osteoporosis
- Prevention of osteoporosis
- When fractures happen
- Fracture management
- Goals and principles of lower limb fracture management
- References
About bones
Bones are living, dynamic organs that are continuously changing and replacing cells, like any other organ in the body, although at a much slower rate.
Different parts of the long bones (Figure 1)
- Shaft or diaphysis.
- Epiphyses, or ends of the bone.
- Proximal epiphysis (the top end of the bone)
- Distal epiphysis (the bottom end of the bone).
- Metaphysis, the area next to the epiphysis.
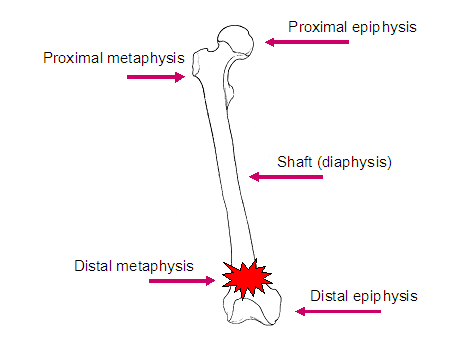 Figure 1
Figure 1
Many of the fractures that individuals with SCI sustain occur in the region of the metaphysis and epiphysis.
Different types of bone (Figure 2):
- Cortical bone, or compact bone, makes up about 80% of bone in the body.
- Trabecular bone is the inner, spongy material and makes up approximately 20% of all bone. Trabecular bone has very high bone turnover, meaning it is formed and reabsorbed at a higher rate than other bone.
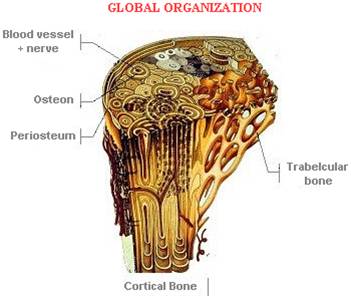 Figure 2
Figure 2
What is osteoporosis?
Osteoporosis, or porous bone, is a disease in which the bones lose density, become weak and brittle, and are more likely to break. In osteoporosis, the normal process of creating new cells and reabsorbing old ones in the bones becomes imbalanced, leading to a gradual thinning of bone tissue. Osteopenia is an intermediate condition in which bone has lost density and strength but has not reached the more fragile state of osteoporosis. You can see this gradual change in Figure 3.
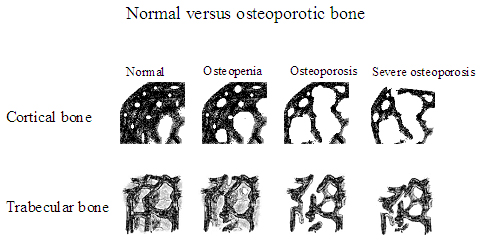 Figure 3
Figure 3
[Images courtesy of Susan Ott, MD, Associate Professor, Department of Medicine, University of Washington.]
Osteoporosis and bone fractures
Bone fractures in the general U.S. population, usually of the hip, are a very disabling and sometimes fatal consequence of osteoporosis; each year, more than 300,000 people over age 65 sustain hip fractures. Of these, 30% die within one year of fracture. Those who survive experience losses in independence and function for a year or two after fracture. After that, only 40% ever regain their former mobility, and only 25% get back their pre-fracture level of independence. The majority (71%) are never able to return to their former living situation.
How is osteoporosis diagnosed?
Bone mineral density is measured using dual-energy x-ray absorptiometry, also known as DXA scanning. The scanner is a padded table with an x-ray tube. The scan gives a score that is compared to that of a healthy person in their 20s. A diagnosis of osteopenia or osteoporosis is based on how far below that ideal a score falls. In the general population, osteoporosis most often shows up in the spine, hip and forearm, so those are the areas that are typically examined with DXA scanning.
Osteoporosis in SCI
While the most common pattern of osteoporosis in the general population is in the post-menopausal female, who classically fractures in the vertebrae, the hips and the wrist, osteoporosis in SCI is quite different.
- In the spinal-cord injured population, osteoporosis has been seen on x-ray as early as six weeks after injury. This decrease in bone mineral density typically levels off around two years after injury. The bone density at this point is about the same as that of a 70-year-old female (without an SCI).
- About 80% of individuals with chronic spinal cord injury have either osteopenia or osteoporosis.
- Bone loss is below the level of injury.
- Most loss is in the trabecular bone in the lower 1/3 of the femur (thigh bone) and upper 1/3 of the tibia (shin bone)—i.e., the areas just above and just below the knee.
- Studies vary, but generally there is about 30% to 40% decrease in bone density in the legs after SCI.
- The lumbar spine maintains normal or higher bone mineral density after SCI. Substantial weight-loading that comes from sitting in a wheelchair may stimulate bone-building activity enough to maintain the bone mineral density in the spine. The non-weight bearing lower extremities don't have this stimulation and therefore lose bone mineral density.
- Injury level
- Individuals with tetraplegia have more areas of bone.
- Individuals with paraplegia usually have bone mineral density preserved in their upper extremities.
- In the bone that is affected, the severity of bone loss is the same both in paraplegia and tetraplegia.
- Extent of injury: Individuals with complete injuries have more bone loss than those with incomplete injuries.
- Spasticity is thought to help maintain bone mass after SCI due to muscle pulling on the bone, similar to the effect of weight-bearing.
- Duration of injury: The longer the time since injury, the greater the bone loss is likely to be.
Causes
In the SCI population, osteoporosis is likely due to many different factors.
- Disuse: lack of mechanical loading on the bone inhibits the stimulation of bone-building cells.
- Disordered vasoregulation: sluggish blood flow to limbs may contribute to a decrease in bone mass.
- Poor nutritional status: inadequate consumption of a healthy, well balanced diet.
- Hormonal alterations (testosterone, PTH, glucocorticoids, calcitonin) that happen as a result of SCI and play a role in the maintenance of bony formation and reabsorption.
- Metabolic disturbances in metabolites and acidity of the blood can influence the balance of bony formation and reabsorption.
- Autonomic nervous system disregulation caused by the injury leads to poor circulation and altered gas and nutrient exchange at the bone.
Screening for osteoporosis in SCI
The goal of screening tests is mainly to identify “silent” disease or risk factors, and sort out the people with and without a certain disease. Screening tests should only be done if care is going to change as a result of the screening. In the able-bodied population, women do not usually start getting bone scans until well after menopause.
Using DXA scanning for people with SCI is controversial and many providers do not recommend it for a variety of reasons. First, it is often difficult to get a good quality DXA scan because of spasticity, contractures, heterotopic ossification (abnormal bone growths), hardware, and previous surgeries. Transferring onto the scanner may be difficult or impossible in some cases.
We already know that most people with SCI have bone loss, and the exposure to radiation that comes from periodic scans may pose an unnecessary risk. If individuals with SCI start on a schedule of scans every year or two starting at a relatively young age (20s or 30s in SCI versus 50s or 60s and older in the non-injured population), the cumulative radiation decades later may be dangerously high. Is it worth it? It’s important for individuals with SCI to talk through the pros and cons of DXA scanning with their physicians.
Since the rate of osteoporosis after SCI is so high, it may be safer to assume that everyone with SCI has the disease rather than doing a screening study just to confirm something that we already suspect.
Treatment for osteoporosis
Pharmacologic treatment
Calcium
- Calcium levels increase suddenly immediately post injury but drop back down after a short period into a new balance of bone building and breakdown.
- Supplementing with calcium alone will not prevent osteoporosis.
- Recommendation is to take 1000-1500 mg/day.
- Calcium carbonate or calcium citrate
- Carbonate is cheaper, but it needs to be taken with meals and interferes with some medications (GI reflux meds).
- Side effects of calcium: renal stones, dyspepsia, constipation, absorption of some meds (thyroid meds and iron).
- Discuss with your provider to determine the appropriate dose for you.
Vitamin D
- Research studies have found that anywhere from one third to nearly a hundred percent of individuals with SCI have either vitamin D deficiency or insufficiency. This is most likely due to a diet too low in vitamin D as well as limited sun exposure because people with SCI often do not get outside enough.
- The standard recommendation for persons with SCI is to supplement with 400-800 IU of vitamin D per day, preferably as cholecalciferol (rather than ergocalciferol).
- For persons with vitamin D deficiency, 2000 IU of oral vitamin D3 with calcium 1.3g daily for 3 months is recommended to safely raise vitamin D levels into normal range.
- There are potential toxic effects of vitamin D, so it is important for each person to discuss dosing with his or her health provider.
Bisphosphonates
- These are drugs that inhibit bone reabsorption and keep the bone from breaking down. Examples are alendronate, risedronate, ibandronate, zoledronate (common names are Fosamax, Actonel, Boniva).
- Some studies have shown bone mass maintenance or even increases in people with SCI, others have shown bone loss or no effect. Any improvements reverse when the drug is stopped.
- Negative side effects after long-term use have been reported recently in studies in the general population.
- We don’t know how safe it is for individuals with SCI to use these drugs for the long-term.
Teriparatide (Forteo)
- This is a synthetic parathyroid hormone.
- There have been no studies of this drug in people with SCI.
- It increased spine and hip bone density in post-menopausal women, but these are not areas at risk in people with SCI.
Non-pharmacologic treatment options
Standing
- Since mechanical loading of the bones can help maintain bone density, many people ask about the use of a standing frame to prevent osteoporosis.
- Results of SCI studies are inconsistent—some showed it maintained density, others showed no benefit.
- There are other benefits of standing, however, such as reduced spasticity, improved range of motion, better mood.
Functional Electrical Stimulation (FES)
- Electrodes are applies to the muscles to produce muscle contraction. This causes muscles to load or pull on the bones.
- Results of studies don’t consistently show whether FES prevents or treats osteoporosis.
- Some studies suggest bone mass is somewhat maintained after FES is stopped. Others found that six months later bone mass returned to what it was before starting FES.
- We don’t know how much FES is needed, or for how long.
- We don’t know if FES actually prevents fractures or in which groups.
Low intensity vibration
- Transmission of low magnitude mechanical signals are delivered by an oscillating platform.
- Maintains bone mineral density in animals and some human studies, but we don’t know why.
- SCI studies are under way now in some centers, but no results yet.
- People with SCI need to use a standing frame with this in order to stand upright enough to put their full body weight on it.
Prevention of osteoporosis
Current state of osteoporosis prevention
- There is no treatment that prevents osteoporosis in non-ambulatory people with SCI at this time.
- When we find treatments that slow bone loss, are they cost effective?
- Multiple medications for life—what are the risks?
- Hours of standing frame or electrical stimulation every week for life—how does that effect quality of life? Is it practical and affordable?
Prevent treatable cause of osteoporosis and fractures
- Consume a healthy diet
- Quit smoking
- Limit alcohol and caffeine intake
- Stay physically and mentally active
- Avoid falls
- Walking or wheelchair—make sure your wheelchair fits and is properly positioned.
- Transfer techniques—make sure your transfers are safe.
- Equipment—use appropriate equipment and keep it well-maintained.
- Environment—make sure the environment (bathroom, bedroom, car, entryways, etc.) allows you to be as safe as possible to avoid falls.
When fractures happen
- Each year, about 2-4% of the SCI population fractures a bone.
- After a fracture heals, there is an increased risk of fracturing the bone at the same place. A broken bone, even when it’s healed, is never as strong as it was before the fracture.
- Most fractures in SCI are at the bottom of the femur or the top of the tibia.
- Only minimal force is required to break a bone after SCI. Frequent causes are:
- Falling from a wheelchair or shower chair.
- Turning in bed or doing range of motion.
- Unknown; the person doesn’t remember anything happening, but notices a leg suddenly becoming swollen. Upon x-ray, a broken bone is found.
Fracture management
Even if a person doesn’t walk, it’s still important to make sure a broken bone heals properly.
- A bone that doesn’t heal correctly can end up deformed, which can lead to medical complications. For example, a pressure ulcer may form at the pelvis or lower limb due to seating changes.
- Deformity may also lead to functional losses that affect independence. If a person’s wheelchair doesn’t fit correctly, he or she may not be able to participate fully in daily or recreational activities.
Goals of fracture management:
- Short term goals:
- Maximize functional independence during fracture healing.
- Minimize complications.
- Modify equipment or provide new equipment.
- Minimize increased caregiver cost.
- Long term goals:
- Minimize deformity.
- Maintain pre-fracture functional abilities.
- Make sure equipment fits properly.
Surgery versus conservative management
Surgery
- The basic principle of surgery is to achieve union of bone in the most anatomic position possible while conserving as much function as possible.
- Surgery is the best management in these cases:
- Displaced fracture
- Unstable fracture
- Femoral neck fracture (hip bone)
- Fracture non-union where prior treatments have failed
- Surgery is not recommended in these cases:
- Osteoporotic bone is too fragile to allow for surgical fixation.
- Active infection of any kind.
- Osteomyelitis (bone infection or inflammation).
Brace options
Fractures can be stabilized with orthotics (splints, braces or casts), but patients with SCI have unique issues to dealt with. Off-the-shelf splints may not fit or work well for SCI patients, so custom-fit devices may need to be fabricated.
Considerations when choosing orthotics:
- Spasticity
- Properly fitting wheelchair.
- Preserving range of motion and mobility skills.
- Skin integrity, edema, and needing to be able to do daily skin checks.
- Ease of taking the brace off and on.
- Effect on the ability to carry on usual activities, work.
- The need for additional caregiver help while healing.
What is the best treatment for people with SCI who break a bone?
Which method results in fewer complications, such as wounds, infection, deep vein thrombosis or pulmonary embolism (DVT/PE), repeat interventions, non-union or poor union of the bone, and even mortality? Other considerations are length of stay in the hospital and whether the person will be able to manage back at home or might need to go to another facility for a while.
Treatment |
Advantages |
Disadvantages |
Conservative/ |
|
|
Surgical |
|
|
A recent VA study in male veterans with SCI found the following:
- No increased risk of death for at least 5 years.
- 70 percent required some sort of equipment changes, at least in the short term.
- At least 50% had reduced functional ability in the short term, requiring more assistance with mobility or routine daily activities.
- Only 17% had reduced functional abilities that lasted longer than one year.
Goals and principles of lower limb fracture management
- Heal fracture with minimal risk of complications.
- Shortening, angulation, and rotational deformities are rarely/never acceptable.
- Consider the reality of the brace (how it will affect daily life).
- Assess all equipment and activities of daily living during and post-fracture healing.
- GOAL: Maintain pre-fracture functional status.
References
- Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and Mortality of Hip Fractures in the United States. JAMA. 2009 Oct 14;302(14):1573-9.
- Koot VC, Peeters PH, de Jong JR, Clevers GJ, van der Werken C. Functional results after treatment of hip fracture: a multicentre prospective study in 215 patients. Eur J Surg. 2000 Jun;166(6):480-5.
- World Health Organization. Assessment of Fracture Risk and its Application to Screening for Postmenopausal Osteoporosis. WHO Technical Report Series 843. Geneva: World Health Organization, 1994.
- Bauman WA, et al. An effective oral vitamin D replacement therapy in persons with spinal cord injury. J Spinal Cord Med. 2011 September; 34(5): 455–460
- Shane E, et al. Atypical subtrochanteric and diaphyseal femoral fractures: Report of a task force of the American Society for Bone and Mineral Research. JBMR. Vol 25 (11). Nov 2010. PP 2267-2294. FDA safety announcement 10/13/10.
- Frotzler A et al. High-volume FES-cycling partially reverses bone loss in people with chronic spinal cord injury. Bone. 2008 Jul;43(1):169-76. Epub 2008 Mar 20.
- Clark JM et al. Physiological effects of lower extremity functional electrical stimulation in early spinal cord injury: lack of efficacy to prevent bone loss. Spinal Cord. 2007 Jan;45(1):78-85. Epub 2006 Apr 25.
- Frotzler A, et al. Effect of detraining on bone and muscle tissue in subjects with chronic spinal cord injury after a period of electrically-stimulated cycling: a small cohort study. J Rehabil Med. 2009 Mar;41(4):282-5.
- Freehafer AA, Mast WA. Lower extremity fractures in patients with spinal cord injury. Jour Bone and Joint Surg. 1965 June;47A-4:683-694.
- Ragnarsson KT, Sell GH. Lower extremity fractures after spinal cord injury: A retrospective study. Arch Phys Med Rehabil. Sept 1981;62:418-423.
- Nelson A, Ahmed S, Harrow J, Fitzgerald S, Sanchez-Anguiano A, Gavin-Dreschnack D. Fall-related fractures in persons with spinal cord impairment: A descriptive analysis. SCI Nursing. 2003;20(1):30-37.
- Canale: Campbell's Operative Orthopaedics 2003. Mosby. Philadelphia, PA.






